Do You Have Diabetes? Here’s Some Eye-Related Information
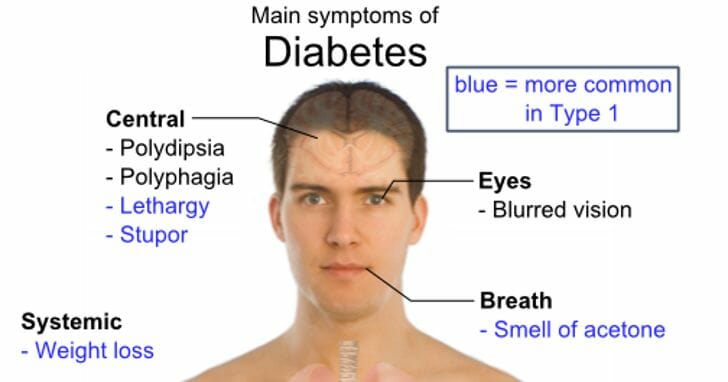
People with diabetes are more prone to developing eye-related conditions and have a higher risk of developing blindness. Diabetes is associated with high blood glucose levels. Over time, high blood sugar levels can be harmful to the eyes, due to an increase in pressure and resulting damage to the blood vessels. Learn more about eye problems linked to diabetes and find out what you can do to prevent or manage these related conditions.
Eye Problems and Diabetes — Glaucoma
Glaucoma involves pressure build-up in the eye, which typically causes slow drainage in the aqueous humor — a protective, fluid-filled anterior chamber through which light enters from the cornea. The slow drainage compromises blood vessels in the retina and optic nerve, causing damage to both and eventually, loss of vision.
Those with diabetes have a 40 percent increased chance of developing glaucoma. Other factors, such as age and length of diabetes diagnosis can increase the risk. Glaucoma treatment may include surgery or medications to reduce pressure.
Cataracts and Diabetes
In cataracts, the lens of the eye blurs and blocks light transmission. Diabetics have a 60 percent higher likelihood of developing cataracts. Diabetes can also cause cataracts to develop more rapidly and much earlier in life.
Depending on the severity of cataracts, it may only be necessary to wear glasses with lenses that reduce glare. However, cataracts can advance to a debilitating loss of vision, which often requires surgical removal of the lens. In some cases, a lens transplant may be possible. In other cases, the process of lens removal can trigger retinopathy, which can also lead to glaucoma.
Diabetes and Eye Problems — Retinopathy
Probably the most common eye condition linked to diabetes is retinopathy, which concerns all eye disorders associated with the retina — the part of the eye that records and transmits images to the brain. A principal cause of adult blindness in the U.S., diabetic retinopathy causes strain on the blood vessels surrounding the retina.
The two main forms are non-proliferative retinopathy and proliferative retinopathy. Non-proliferative retinopathy causes mild, moderate or severe blood vessel blockage in the back of the eye. Macular edema is the most serious type of non-proliferative retinopathy and can cause blurred vision and vision loss if left untreated.
Proliferative retinopathy is the less common, acute form of retinopathy. Proliferative retinopathy is usually the result of severely progressed blood vessel damage, to such a degree that the vessels close off, causing the formation of weaker blood vessels and leading to hemorrhaging, scar tissue, and ultimately, vision loss and detached retina. Once the condition has progressed to the point of retinal detachment, proliferative retinopathy can be extremely difficult to treat.
Symptoms associated with diabetic retinopathy may include pressure in the eyes, difficulty with peripheral vision, double vision, blurring, dark spots and light flashes.
Retinopathy risk factors include genetics, blood pressure and blood sugar issues and length of time living with diabetes.
Preventive Measures for Diabetes and Eye Health
Eye problems associated with diabetes are typically minor. However, because of the propensity, diabetic patients should schedule regular eye exams to safeguard vision and health of the eyes. To manage diabetic retinopathy, an annual eye exam is necessary to monitor and prevent the progression of the disease.
[Photo Credit: Salem Free Med Clinic]