Understanding Diabetic Retinopathy
The number one cause of blindness in the United States results from diabetes. Diabetes causes problems in the way the body uses sugar, and it can create changes in veins, arteries, and capillaries that carry blood throughout the body — including the eyes. There are a variety of diabetes-related eye diseases like glaucoma, cataracts, and diabetic retinopathy, which affects the retina and can potentially lead to vision loss.
Diabetic retinopathy (DR) affects over 85% of people with Type 1 diabetes and approximately 40% of Type 2 diabetes sufferers in the United States. While diabetic retinopathy is the primary cause of blindness in adults in the U.S., with early detection, it can be treated and the risk of blindness can be greatly reduced.
Causes of Diabetic Retinopathy
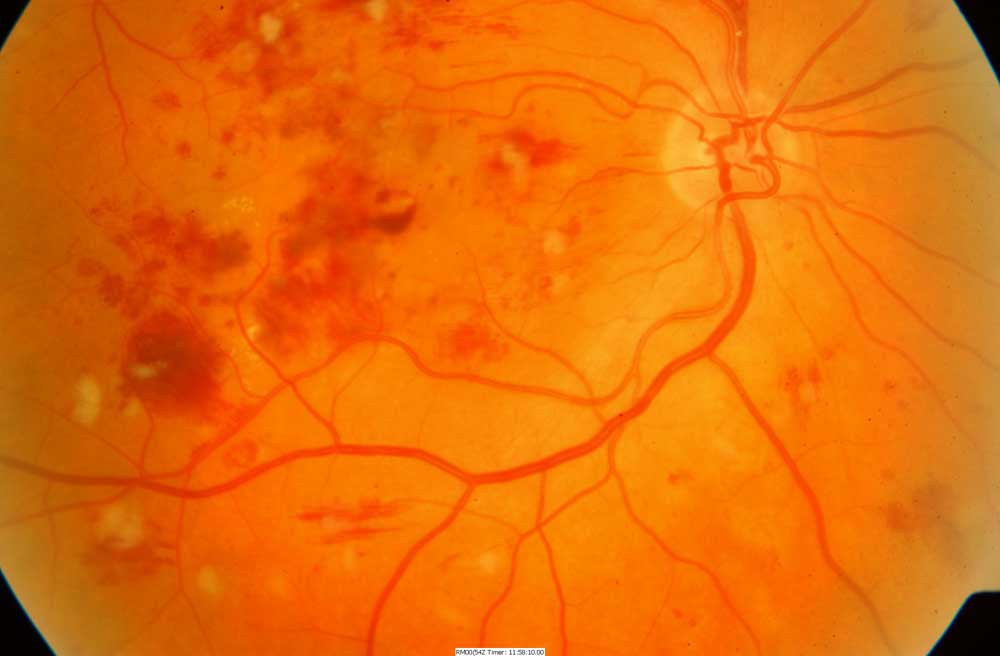
People with diabetes over time can develop buildup in their blood vessels, which causes blood flowing to the eyes to slow. Eventually the retina will start releasing chemicals in attempts to open up the vessels to get the blood flow it needs. Problems begin to arise when the retina begins to start producing an overabundance of weak blood vessels to compensate, as these weaker vessels can obstruct and blur vision to varying degrees either by their abundance, or by their rupture and leakage.
Different Types of Diabetic Retinopathy
The retina is a lining at the back of the eye that captures light and transfers it into information that gets sent along the optic nerve to the brain. In the center of the retina is the macula, which is primarily responsible for sharp, clear images.
There are two types of diabetic retinopathy that can both affect a person’s vision: the first is diabetic macular edema, which occurs when blood vessels around the macula in the central retinal area leak. In turn, this affects the eye’s ability to clearly capture light, and to transfer it into information for the brain. The most common result of diabetic macular edema is mild to moderate blurred vision. This type of diabetic retinopathy is the more common problem associated with vision problems.
The second and less common is proliferative diabetic retinopathy, which tends to be a more severe and advanced form of diabetic retinopathy. Proliferative diabetic retinopathy is characterized by large amounts of new and relatively weak blood vessels growing on the retina. These vessels are extremely susceptible to rupture and can bleed into the gel that fills the eye, blocking vision. These ruptures can eventually for scar tissue on the retina, causing it to shrink and pull, and may result in a traction retinal detachment.
Treatment and Outcomes
The key to treating diabetic retinopathy is early detection and treatment. Optometrists can test for the disease and if detected, current treatment procedures can lead to stabilization and prevention of loss of sight for many people.
[Photo Via: Virginia Retina]

